Do federal employees go on Medicare?
Unfortunately, federal employees do not receive free health insurance in retirement. However, federal employees can keep their current FEHB (federal employee health benefits) plan after retirement. … The government pays the remainder of the pension premium at the same rate as for current employees.
Can I keep my FEHB after age 65?
Contents
Your FEHB coverage will continue whether or not you enroll in Medicare. If you can get paid Part A coverage, we recommend that you sign up for it. Most federal employees and annuitants are entitled to Medicare Part A at age 65 at no cost. … If you don’t enroll in Medicare, your FEHB plan pays for benefits in full.
Can I remain insured after my 65th birthday? If you receive employer-sponsored health insurance through you or your spouse’s job when you turn 65, you may be able to keep your insurance until you (or your spouse) retire.
How long can I keep FEHB in retirement?
Most employees are aware of this five-year rule; however, they’re not clear on what that five-year rule really means. It does not mean that the employee had to be in the same FEHB subscription for five years. Employees are allowed to change carrier, plan, and type of coverage within that five-year period.
How does FEHB work after retirement?
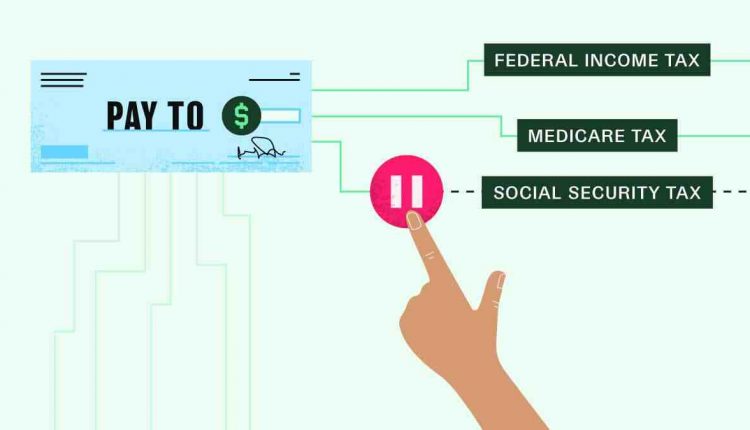
Once employees retire and have chosen to keep their FEHB coverage after retirement, they start paying the premium with after-tax cash. While they work, they pay the FEHB premium with pre-tax money, but when they retire, they pay it with after-tax money.
Do federal employees get medical benefits when they retire?
After retirement, federal employees enjoy a monthly annuity and medical coverage. To qualify for coverage, you must meet minimum service requirements, which include being covered as a federal employee for at least five years. Your spouse will receive coverage without the five-year plan.
Should I keep my FEHB after age 65?
It is imperative that a federal employee retiring from FEHB enroll in Medicare Part A and opt for Part B, C, or D coverage. Minor children under age 26 do not lose their health insurance. However, this is only if you enroll in Medicare and remain enrolled as an FEHB.
Is Medicare Advantage better than FEHB?
Most MA plans are similar to FEHB plans in hospital and medical benefits, but the benefits of prescription drugs will not be as good as in the FEHB program because the plans have a coverage gap where you are responsible for all or most drug costs until you reach a catastrophic limit.
Do I need Medicare B if I have FEHB?
If you work and have FEHB or if you are covered by your spouse’s group health insurance plan, you do not need to enroll in Part B when you turn 65. You have a special enrollment period when you retire or your spouse retires to enroll in Part B without paying a penalty.
Should I keep FEHB when I retire?
Keeping FEHB in retirement is very important Being able to retire FEHB gives you more flexibility in your retirement planning. You will retain better coverage at a lower cost, and the government will continue to pay the bulk of your premium costs.
Are you automatically signed up for Medicare Part B?
Medicare automatically enrolls you in Part B. Your Medicare card will be mailed to you approximately 3 months before your 65th birthday. If you’re not getting disability benefits and Medicare when you turn 65, you’ll need to call or visit your local Social Security office, or call Social Security at 1-800-772-1213.
Is Medicare Part B Free When Disabled? Most people who receive Social Security benefits do not have to pay for Medicare Part A. … Most people who receive Social Security benefits do have to pay a premium for Medicare Part B, but you can choose to opt out of this program if you already have health insurance.
Can you enroll in Medicare Part B anytime?
If you did not enroll in Part B during your initial enrollment period, you may be eligible for a Special Enrollment Period (SEP) at any time to enroll in Part B (and/or Part A) as long as you or a spouse works and you are covered by a group health plan through that employment.
Is there an enrollment period for Medicare?
If you miss your first opportunity, you generally have to wait until fall for Medicare’s annual Open Enrollment Period (October 15 – December 7) to participate in a plan. Each year during this time, you can also stop or change your subscription coverage.
Can you enroll in Medicare anytime?
Initial Enrollment Period – If you become eligible for Medicare when you turn 65, you can enroll during your initial enrollment period. …You can sign up for free Medicare Part A (hospital insurance) (if you qualify) anytime after your initial enrollment period begins.
What is the difference between FEHB and Medicare?
your FEHB plan is the primary payer of the cost of health benefits and Medicare is the secondary payer if you are employed by the federal service; Medicare is the primary payer and FEHB is the secondary payer if you are not employed by the federal service.
Can Federal Employees Have Both FEHB and Medicare? The answer: yes! FEHB coverage is similar to Medicare coverage. … Federal employee plans often include prescription drug benefits, although drug coverage may vary. As with any prescription drug plan, check for specific medications on the plan’s formulary.
Is Medicare Advantage better than FEHB?
Most MA plans are similar to FEHB plans in hospital and medical benefits, but the benefits of prescription drugs will not be as good as in the FEHB program because the plans have a coverage gap where you are responsible for all or most drug costs until you reach a catastrophic limit.
Is Medicare Advantage a federal health care program?
Medicare is a federal health insurance program regulated by the Centers for Medicare and Medicaid Services (CMS).
Is Medicare Advantage creditable coverage?
Medicare Advantage plans must offer benefits at least as comprehensive as Medicare Parts A and B. That’s why all Medicare Advantage plans have creditable coverage.
Is Medicare federal health insurance?
Medicare is the federal health insurance program for: People age 65 or older. Certain young people with disabilities. People with end-stage kidney disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Is Medicare Part B federal program?
Medicare is a federal health insurance program for people age 65 or older, people under age 65 with certain disabilities, and people of any age with end-stage renal disease.
What type of insurance is Medicare?
Medicare is the federal government’s program that provides health care (health insurance) coverage if you are age 65 or younger and receive Social Security Disability Insurance (SSDI) for a specified period of time, or under age 65 and with End-Stage Renal Disease (ESRD ). ).
Do I need both FEHB and Medicare?
Answer #1 —You don’t need both. In many cases, FEHB appears to be more comprehensive, often including emergency care outside of the US, as well as dental and vision, which Medicare does not cover.
How do you qualify for $144 back from Medicare?
How do I qualify for the refund?
- Be a Medicare beneficiary enrolled in Part A and Part B,
- be responsible for paying the Part B premium, and.
- Live in a service area of a plan that has chosen to participate in this program.
What is the Medicare Give Back Program? The refund benefit is another term for Part B premium reduction. This is when a Medicare Advantage plan reduces the amount you pay for your monthly Part B premium.
How does Medicare Part B reimbursement work?
The Medicare Part B Reimbursement Program reimburses the cost of eligible Medicare Part B benefits of retirees using funds from the retiree’s Sick Leave Bank. Medicare Part B benefits are not taxable for the retiree.
How do I get my $144 back from Medicare?
You must be enrolled in a Medicare Advantage Plan To enroll in a Medicare Advantage Plan, you must be enrolled in or eligible for both Medicare Part A and B. To receive the Medicare refund benefit, you must enroll in a plan that offers to pay your Part B monthly premium.
How does Medicare reimbursement account work?
Medicare Reimbursement Account (MRA) Basic Option members who pay Medicare Part B premiums can be reimbursed up to $800 per year! You must submit proof of Medicare Part B premium payments through the online portal, the EZ Receipts app, or by fax or mail.
Who qualifies for Medicare money back?
Who doesn’t love getting a refund? Each year, Basic Option members enrolled in Medicare Part A and Part B can get money back into their bank account. The Blue Cross and Blue Shield Service Benefit Plan reimburses these members up to $600 per calendar year for their Medicare Part B premium payments.
Does Medicare give back money?
The Medicare Giveback benefit is a Part B premium reduction offered by some Medicare Part C (Medicare Advantage) plans. If you enroll in a Medicare Advantage plan with this benefit, the plan carrier pays some or all of your monthly Part B premium.
How can I get money back from Medicare?
Each year, Basic Option members enrolled in Medicare Part A and Part B can get money back into their bank account. The Blue Cross and Blue Shield Service Benefit Plan reimburses these members up to $600 per calendar year for their Medicare Part B premium payments.
How do I get my $144 back from Medicare?
You must be enrolled in a Medicare Advantage Plan To enroll in a Medicare Advantage Plan, you must be enrolled in or eligible for both Medicare Part A and B. To receive the Medicare refund benefit, you must enroll in a plan that offers to pay your Part B monthly premium.
What is Medicare gift back?
What is the Give Back Benefit in Medicare? The refund benefit is another term for Part B premium reduction. This is when a Medicare Advantage plan reduces the amount you pay for your monthly Part B premium.
Who is eligible for Medicare reimbursement?
Only the member or a qualifying survivor/resident partner enrolled in Part A and B is eligible for Medicare Part B premium reimbursement.
How much does FEHB cost after retirement?
FERS retirees must choose 50% or 25% survivor’s annuity for your spouse to qualify for FEHB coverage upon retirement after the annuitant’s death. The 50% election will cost you 10% of your full annuity and the 25% survivor’s annuity election will cost you 5% of your full annuity upon retirement.
What is the cost of FEHB for retirees? For retirees and non-postal workers in the largest FEHB plan, Blue Cross/Blue Shield standard, the biweekly self-only enrollment rates increase by $6.54 to $123.45, self-plus one by $13.66 to $280.81 and for family coverage with $13.38 to $300.12.
What happens to my FEHB when I retire?
Once employees retire and have chosen to keep their FEHB coverage after retirement, they start paying the premium with after-tax cash. While they work, they pay the FEHB premium with pre-tax money, but when they retire, they pay it with after-tax money.
Does health insurance continue after retirement?
Can I keep my healthcare allowance after my retirement? Yes, you can keep your existing health coverage if you meet all of the following conditions: You are enrolled in federal health insurance plans when you retire.
Do federal employees get healthcare for life?
When you start working for the federal government, retirement benefits are part of the package. This includes a monthly annuity, which pays you part of your salary from the moment you retire until your death. In addition to this annuity, you are entitled to medical benefits, including health, eyesight and dentistry.
How much does FEHB cost per month?
The monthly maximum government contribution (72% of the weighted average) is $530.53 for Self Only, $1,136.70 for Self Plus One, and $1,243.95 for Self and Family.
Why is FEHB so expensive?
There are a number of reasons why having FEHB is so rare and valuable. First, few employers offer comparable coverage. … This means that if you pay $400 per month in FEHB premiums, the total premium cost will be approximately $1,400 per month. It would cost a lot more than that to find comparable coverage on your own.
Do you pay for FEHB?
You must pay both the government and the employee share of the costs. Premium conversion is a method of reducing your taxable income by the amount of your FEHB insurance premium.
How do I opt out of Part B?
Cancel Medicare Part B. The Part B cancellation process begins by downloading and printing Form CMS 1763, but do not complete it yet. You must complete the form during a telephone or in-person interview with a representative of the Social Security Administration (SSA).
Is it mandatory to buy Medicare Part B? Medicare Part B helps cover medical services such as doctor’s services, outpatient care, and other medical services that Part A does not cover. Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary.
What happens if I don’t want Medicare Part B?
If you didn’t get Part B when you first became eligible, your monthly premium could increase by 10% for every 12-month period you could have had Part B but didn’t sign up for. In most cases, you will have to pay this penalty every time you pay your premium, as long as you have Part B.
Can I refuse Part B Medicare?
Once you’ve applied to receive Social Security benefits, you can only defer your Part B coverage; you cannot defer your Part A coverage. To defer Part B, you must decline Part B before your Medicare coverage begins.
Can you opt out of Plan B?
Yes, you can opt out of Part B. (But make sure your new employer insurance policy is “primary” for Medicare. … Medicare is pushing for an interview to make sure you know what the consequences will be if you don’t part B steps”. €” for example that you may have to pay a late fine if you want to re-enrol for the course in the future.
Can you have Medicare Part B without Part A?
While it is always advisable to have Part A, you can purchase Medicare Part B (medical insurance) without having to purchase Medicare Part A (hospital insurance), as long as you are: 65 years of age And a U.S. citizen or legal resident who has at least five years in the US.
Can I stop my Medicare Part B?
You can voluntarily terminate your Medicare Part B (health insurance). However, as this is a serious decision, you may need to have a face-to-face meeting. A Social Security representative will assist you in completing Form CMS 1763. … You may also contact the nearest Social Security office.
Can I stop my Medicare Part B?
You can voluntarily terminate your Medicare Part B (health insurance). It’s a serious decision. … You must have a face-to-face meeting with Social Security before you can terminate your Medicare Part B coverage. Call the SSA or your local Social Security office to schedule your interview.
What happens if you opt out of Medicare Part B?
Canceling Part B Because You Were Automatically Enrolled But Beware: If you opt out of Part B without proper coverage — that is, employer-sponsored health insurance from your current job that’s as good or better than Medicare — you can you are late – enrollment fines (LEPs) down the line.
Can you stop taking Medicare Part B?
You can voluntarily terminate your Medicare Part B (health insurance). However, as this is a serious decision, you may need to have a face-to-face meeting. A Social Security representative will assist you in completing Form CMS 1763. … You may also contact the nearest Social Security office.
Comments are closed.